Is your job putting you at risk of a heart attack?
As you can imagine, this question has preoccupied epidemiologists and public health specialists for decades. But despite years of research, straightforward or clear answers are not always available for specific job descriptions. The medical literature is usually guarded in its assessment of occupational factors leading to heart disease.
Also, if a certain job is linked to an increased risk of heart disease, the job itself may not be the cause of the problem. For example, risk factors for heart disease (such as smoking) may be more common in certain occupations than in others, making it seem like the job itself imparts the risk.
With this in mind, below are 8 findings that have emerged from years of research:
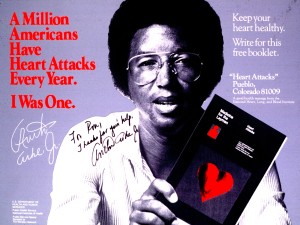
Image attribution: National Institutes of Health, Licensed under Public Domain via Wikimedia Commons
1. NO JOB IS SAFE. It has been apparent for a long time that no job or profession will fully protect someone against heart disease. As we have seen previously, even professional athletes can develop coronary disease at a relatively young age. A sad example that older readers will remember is the case of tennis champion Arthur Ashe who had his first heart attack at age 39, following which he underwent 2 coronary bypass surgeries (he contracted HIV during the second surgery and died of AIDS at age 50).
Premature coronary disease occurs among successful CEO’s, Hollywood stars, doctors, scientists, and religious monks. And if you think that the condition of working is itself the problem, don’t be so sure: heart disease is even more common about the unemployed seeking work and those out of the labor market altogether.
2. SERVICE WORKERS AND BLUE COLLAR WORKERS ARE WORSE OFF. According to annual surveys by the Center for Disease Control (CDC), coronary heart disease and stroke are about 50% more common among blue collar workers and service workers (e.g., hairdressers, nurse aides, cooks) than among white collar workers. For farm workers the prevalence of coronary disease is in-between that of the blue and white collar workers.
The increased prevalence of cardiovascular disease among service and blue collar workers is likely due to the higher prevalence of risk factors such as smoking, high-blood pressure, and diabetes, but there may be other reasons as well. Even if one adjusts for the prevalence of risk factors, socioeconomic conditions still play a role. This was demonstrated in the famous Whitehall study of British civil servants which showed that lower socioeconomic status conferred an increased risk of cardiovascular mortality even when known risk factors (such as blood cholesterol, smoking, etc.) were taken into account.
Interestingly, this situation is the reverse of what was happening at the beginning of the heart disease epidemic. In the first part of the 20th century, coronary disease was commonly felt to be a disease of the rich and upper class.
3. FIRE-FIGHTERS ARE AT VERY HIGH RISK. The incidence of sudden cardiac arrest seems to be particularly high among fire-fighters. In fact, one half of on-duty fatalities among firefighters are due to sudden cardiac arrest rather than fire injury. As it turns out, firefighters seem to have a high prevalence of coronary risk factors, but other factors such as the sudden high stresses with sudden bursts of activities, night-shift work, and other difficult lifestyle conditions likely play a role. The prevalence of coronary disease among firefighters is so high that more intensive cardiac screening is increasingly being recommended. We will have an opportunity to discuss the situation of fire-fighters and police officers in more detail in a future post.
4. WORK STRESS IS A FACTOR…Maybe. Several studies have shown that self-assessment of job stress is associated with future risk of cardiovascular complications, but others have not. Stress is an elusive concept that does not lend itself easily to research methodology. The latest findings seem to indicate that if work stress is a factor, the magnitude of the effect is not very high.
Intuitively, we want to believe that job stress has a negative impact on cardiovascular health but this presupposition may bias the research. In fact, some scientists have recently shown that research studies which claim that job strain contributes to heart disease tend to be more popular among epidemiologists than those studies which show no correlation between job strain and heart disease, even if the latter are more rigorously conducted than the former.
But don’t get me wrong, I am not saying that self-perceived job stress is benign or should be ignored!
5. ADMINISTRATORS, RESTAURANT WORKERS AND TRAVEL AGENTS BEWARE! The latest CDC report on heart disease among workers aged less than 55 years identified two industry categories where the prevalence of coronary disease was highest: Administration and Support and Waste Management and Remediation Services and Accommodation and Food Services. If you are scratching your head trying to decide if your company fits one of these categories, you are probably not alone. One of the problems with CDC surveys is that they rely on government industry codes and classifications that were designed for socioeconomic but not medical purposes. Therefore, jobs are lumped together that have substantially different working conditions.
Be it as it may, the Administration category includes business that provide administrative and business support, travel and reservation services, security services, and waste management services, whereas the Accommodation category includes establishments that provide lodging or serve food. In both of these industry groups, the prevalence of coronary disease was 40% more than in the other industries taken as a whole. In this CDC study, there was no adjustment made for the prevalence of known risk factors (such as smoking, high blood pressure, etc.).
6. PHYSICALLY-DEMANDING JOBS MAY BE A PROBLEM. We all know that lack of physical activity is very detrimental for cardiovascular health. This has been demonstrated in numerous studies, leading to strong public health recommendations that everyone engage in some level of physical activity routinely. The main caveat is that this truth concerns leisure-time physical activity such as exercise and sports, or activity that one may do during a lunch break at work, such as walking, or on the commute to and from work.
I frequently encounter patients who perform heavy physical activity as part of their job and who believe that they derive cardiovascular benefit. Unfortunately they are probably incorrect. Moderate to heavy physical activity that is part of one’s job, like lifting heavy loads or operating heavy machinery does not have the same beneficial effect as leisure-time activity, and some recent studies (see here and here) indicate that occupational efforts may actually be harmful to the cardiovascular system.
7. SHIFT WORK IS A CONCERN. Epidemiologists have observed an association between shift work and heart disease but, as in the case of job strain, the results are not always consistent across studies, and to this day it is unclear to what extent shift work plays a role in causing or worsening coronary disease. Part of the difficulty is that shift work can be occasional, frequent, fixed or rotating. Studies don’t always make the distinction. A recent prospective study of Japanese workers, for example, showed that rotating-shift work was associated with an increased risk of heart disease, but that fixed night-shift work was not.
The suspicion is that rotating shift work is particularly taxing on the body, interfering with normal functioning of the hormonal and immune systems, which may in turn have adverse effects on the heart.
8. OCCUPATIONAL EXPOSURES ARE NOT A HIGH RISK. The CDC lists 3 occupational chemicals which are known to have effects on the heart: carbon disulfide (used as an industrial solvent, in fumigation and insecticides), carbon monoxide (present in motor exhaust), and nitroglycerin (used in the munition industry).
Other chemicals affect the heart indirectly by affecting the lungs first. For example, exposure to beryllium (used in aerospace manufacture) can cause scarring of the lung tissue which, in turn, can put stress on the heart. By now, in the United States, many of the known lung exposures are minimized
There is also some indication that occupational noise can increase blood pressure, which could have deleterious cardiovascular effect in the long term.
According to the CDC, studies linking chemical exposure to the development of heart disease have been mixed. In general, when occupational exposures are linked to heart disease, the magnitude of the effect seems to be small.
TAKE HOME MESSAGE:
As we have seen from this summary of the research, occupational factors can potentially play a role in the development or progression of cardiovascular disease. This is not surprising, since our jobs are an intimate part of our lives.
But overall, what seems to be clear is that personal health habits are much more important than work conditions and can largely overcome any added risk from our jobs. Since many of us do not have the luxury of being able to modify our work conditions at will, let’s focus on what we do outside of work as the best way to ensure a healthy future: exercise regularly and eat healthy foods in moderation. In addition, we also invite you to consider a state-of-the-art comprehensive cardiovascular screen, since cardiovascular disease usually lurks before it strikes.
I hope you have found this article informative. If you are interested in the content we provide, make sure you sign up for our free monthly newsletter, which includes our best blog posts and additional pratical information on heart health and sports cardiology news. The sign up form is in the footer at the bottom of this page.
Dr. Accad